Whether you’re living with CIDP (chronic inflammatory demyelinating polyneuropathy) or you’re a caregiver of a loved one with CIDP, managing your day-to-day schedule around symptoms and treatments can become challenging. Your days may include CIDP treatment appointments, office visits with specialists, errands to run, plus family and friend obligations. But as you know, CIDP doesn’t take a day off.
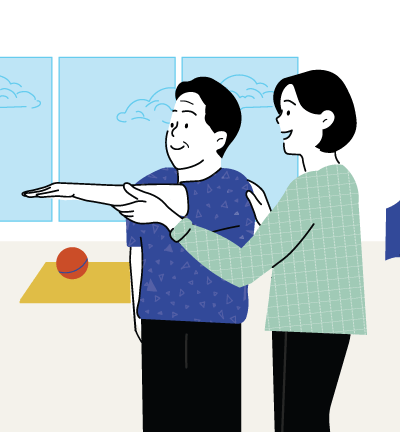
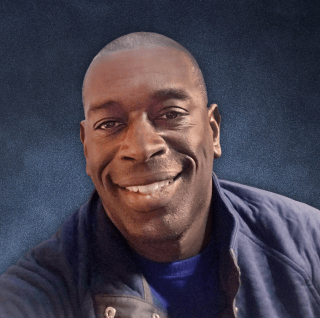
That’s why we talked with people who live with CIDP and their caregivers—Rorey, Doug, Marcy, and Paula—to gather practical time-management tips that may help you better plan your days while living with CIDP.

Finding a CIDP treatment that works for your schedule
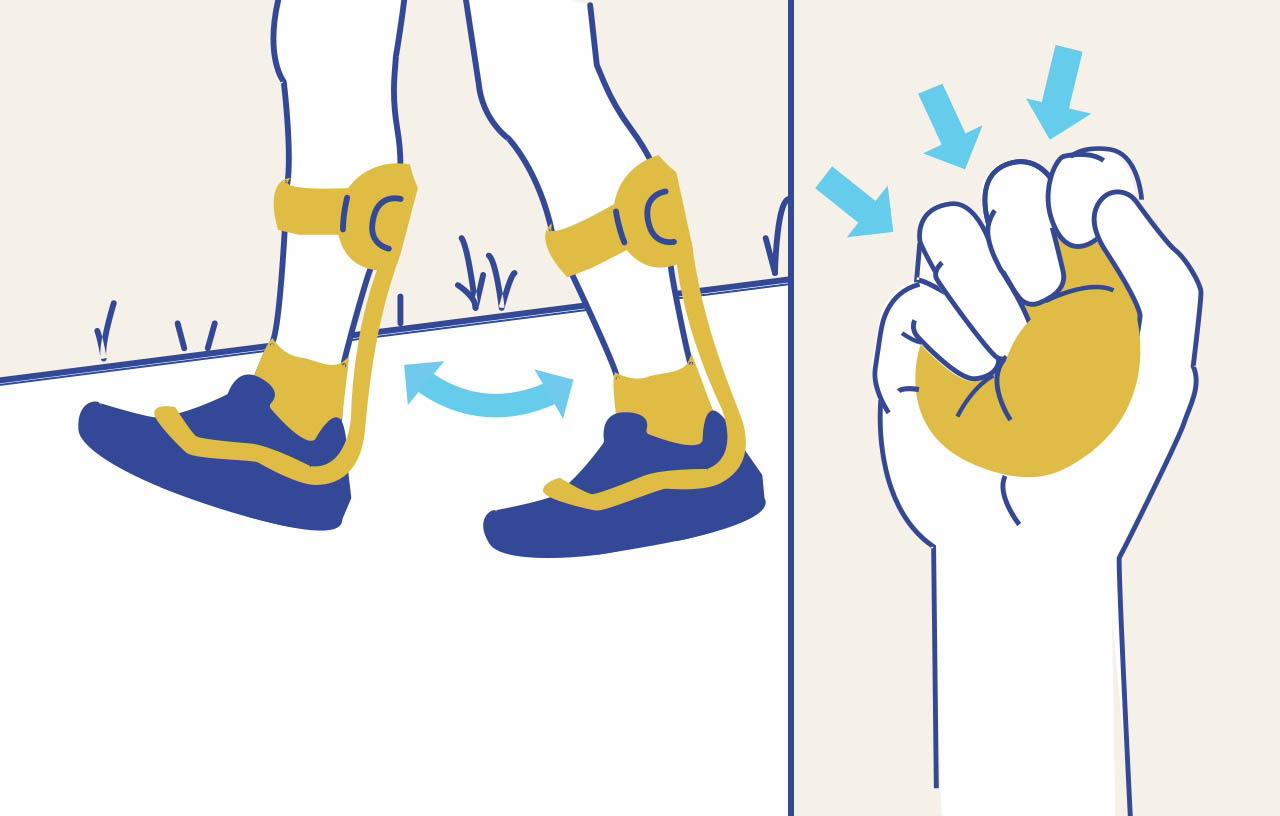
When researching CIDP treatment options, consider how the treatment is given, how often it’s received, and whether it fits with your daily routine, essential tasks, must-have moments, and personal needs. Use this doctor discussion guide to help you and your doctor determine what treatment may be right for you or your loved one’s needs.
Keeping a calendar to stay organized
Whether you prefer a physical planner or a digital calendar, tracking doctor appointments or daily activities may help you stay organized and on top of your schedule. For Doug, a busy family man and caregiver to his wife, Mel, who lives with CIDP, their digital calendar is essential for managing time: “Everything is shared in a digital calendar with invitations, reminders, and any details we can include.” Through consistent communication and planning, they manage their family’s hectic schedules and still make time for each other.
Rorey, who lives with CIDP, used to be highly organized and was never late to appointments before his CIDP diagnosis. After he was diagnosed, he found himself stressed because of the number of doctors’ appointments, and he struggled to remember them all. “I started putting my doctors’ appointments on my work and personal calendars right away—that way, I don't miss it.”
Developing a routine
Living with CIDP often comes with challenges like fatigue or muscle weakness, but many people living with CIDP and their caregivers develop routines to help navigate around these symptoms. For Rorey, it’s imperative for him to have a routine to plan for his week. On Sundays, if his energy allows, he uses the day to prepare for the week ahead by meal prepping and utilizing a pill organizer for his medications. He explained, “Just doing that has helped me a lot, so I’m not scrambling around.”
Marcy, a caregiver for her husband, Rick, who lives with CIDP, shared that their plans typically depend on how Rick feels after his CIDP treatments. She mentioned that they “usually plan everything around those appointments.”

However, routines aren’t everyone’s strong suit. If you struggle sticking to a consistent routine, you can use methods like “backwards planning,” which is Doug’s go-to when it comes to planning his day. With this method, he noted it’s important to consider how much time everything takes and then plan backwards to know when you need to start your day. He explained, “Backwards planning is something I learned when I was in the military and have always leaned on, especially as I've gotten older.”
Making trips easier
When living with CIDP, time management can be important for maintaining your energy throughout the day. When Paula goes grocery shopping, she plans a list ahead of time so she’s not missing items or backtracking down the aisles. For daily errands, Paula said, “I try to make sure where I'm going in town is all in the same area. I don't want to be zigzagging all over town.”
If Rorey is running errands, he stays conscious of his energy levels and when he might need to break up certain errands to avoid tiring himself. “If I know I have a list that's going to take me longer than a half an hour, I either have to break it up or I need to order some things online, because that's not going to work for me.” Online shopping or using grocery delivery apps may be a helpful alternative for those who aren’t able to leave the house as often.
Overall, having a plan for how you handle everyday errands saves time so you can have more energy to do the things that bring you joy.
Being flexible and giving yourself grace
Routines, reminders, and scheduling tools can be helpful with time management, but remember to be kind to yourself—whether you live with CIDP or you’re a caregiver. Remind yourself that it’s okay to modify your routine and allow flexibility in your day-to-day.
When it comes to scheduling plans with friends or family, people living with CIDP may need to wait until the day of, in order to see how their CIDP symptoms are affecting them. Marcy mentioned, “There has to be a lot of flexibility. Sometimes, I just need to go and do things without him, which I don't do too often because I feel a bit guilty.” For Marcy’s husband, Rick, it’s all about pacing himself throughout the day to conserve his energy. “If he's feeling better one day, we'll do a little more. But we know that the following day, we'll do a little less because he’ll likely be tired.”
As a caregiver, Doug talked about how communication is key in his family—whether that’s leaving sticky note reminders for each other, texting about the grocery list, or even picking up on nonverbal cues. For example, if his wife is sleeping, he lets her rest and will take care of the household chores without her needing to ask him. “You have to just be realistic about what you can get accomplished on any given day, and you have to stay positive about the things that you can still do,” he shared.
Don’t be afraid to ask for help
When others don’t fully understand this condition, it can feel difficult to reach out to friends or family for extra support. However, having a strong support system for CIDP—whether it’s a broad circle or just a few trusted people—may help ease your stress and manage your time more effectively.
Consider talking with your employer about any work accommodations that might be needed. Doug informed his employer of his responsibilities as a caregiver for Mel and his personal medical needs, so if he needed to leave early or change his schedule, they would be aware of his situation.
Learn about your rights under a federal law known as the ADA (Americans with Disabilities Act). State laws may provide additional protections.

Building a sense of community can be incredibly valuable when it comes to asking for help. Connecting with others who are also living with CIDP—or caregiving for someone with CIDP—can provide a supportive space, whether it's in person or online. As Marcy shared, “Rick is online a lot, talking to other people that have CIDP, figuring out how to help other people with CIDP.” If you’re looking to get more connected to the CIDP community, check out the GBS | CIDP Foundation International.
Takeaways
- Using a physical or digital calendar helps with daily tasks like setting CIDP treatment appointments and managing your time
- Developing a routine may help you better plan time around symptoms
- When running errands, try to group together tasks that are near each other to avoid overexerting your energy
- Remember to stay flexible when it comes to planning and to give yourself grace
- Sometimes, asking for help from a family member, friend, or even explaining your medical needs to your employer may help with managing your time